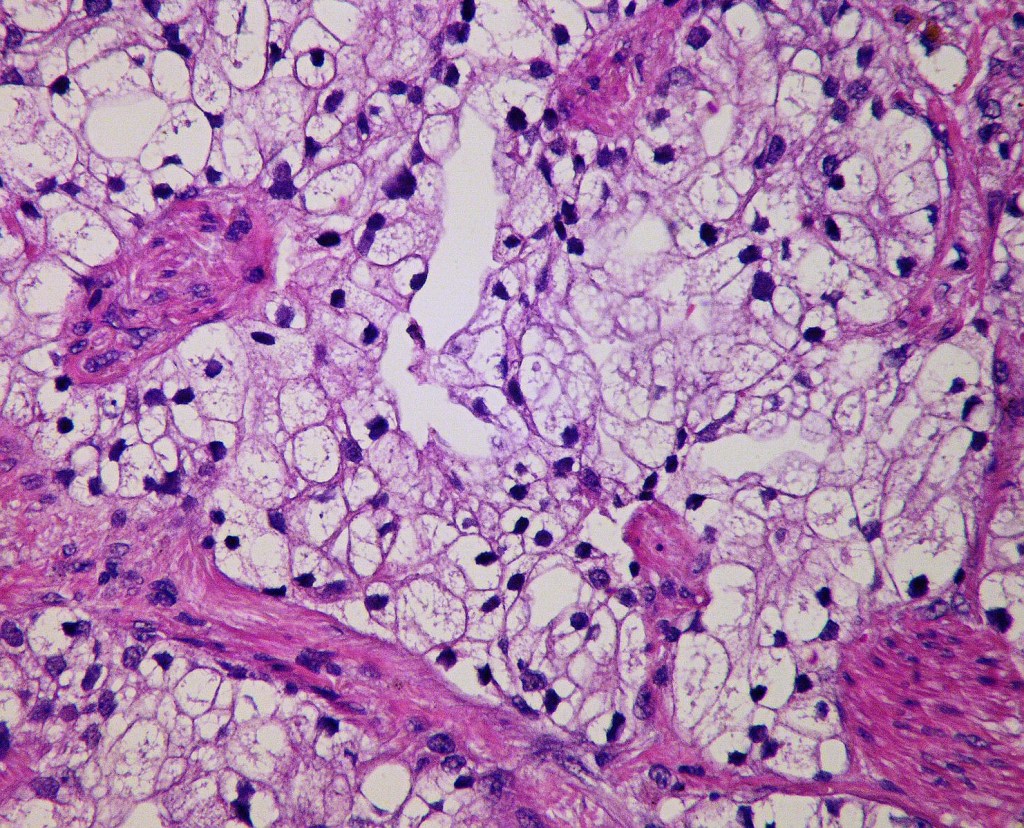
Prostate cancer can be treated with curative intent if it is localised to pelvis.
But in patients with high risk cancers, additional treatments might be needed to improve the odds of controlling the cancer.
Abiraterone is one such add-on treatment that has been shown to improve long term outcomes in a large UK trial.
Unfortunately the drug, abiraterone, even though it is much cheaper now, is not widely available in the UK National Health System ( NHS).
Now an AI (artificial intelligence) test has been developed which selects better those patients who are likely to benefit from Abiraterone.
Hopefully the test will become available for routine use in the near future.
The study data was presented at the prestigious annual meeting of the American Society of Clinical Oncology (ASCO) at Chicago.
Dr Sundar is a member of American Society of Clinical Oncology (ASCO) and has been a member for more than 25 years.
References
BBC news. Hugh Pym and Ian Atkinson. Men denied life-extending prostate cancer drug
UCL. AI test to determine best prostate cancer treatment could save lives and money. 30 May 2025.
Daily Telegraph. Give prostate cancer patients drug that halves risk of death, NHS told.

Disclaimer: Please note – This blog is NOT medical advice. This blog is NOT a expert medical opinion on various topics. This blog is purely for information research only and do check the sources where cited. Please DO consult your own doctor to discuss concerns and options, which are relevant and specific to you. The views expressed in this blog are NOT, in any way whatsoever, intended to be a substitute for professional advice. The blog is NOT previewed, commissioned or otherwise endorsed, in any way, by any organisation that the author is associated with. The views expressed in this blog likely represents some of the author’s personal views held at the time of drafting the blog and MAY CHANGE overtime, particularly when new evidence comes to light.